Health/Medical
See other Health/Medical Articles
Title: Marijuana Use and PTSD among Veterans
Source:
ptsd.va.gov
URL Source: https://www.ptsd.va.gov/professiona ... arijuana_use_ptsd_veterans.asp
Published: Oct 30, 2017
Author: Marcel O. Bonn-Miller, Ph.D. and Glenna
Post Date: 2017-10-30 08:11:42 by Gatlin
Keywords: None
Views: 6775
Comments: 39
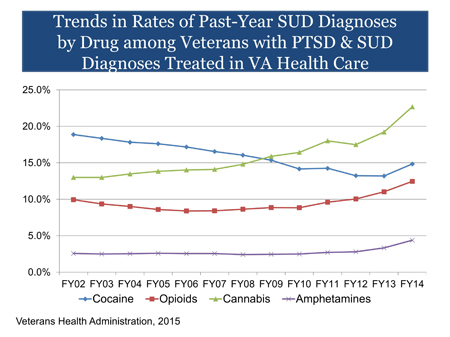
Marijuana use for medical conditions is an issue of growing concern. Some Veterans use marijuana to relieve symptoms of PTSD and several states specifically approve the use of medical marijuana for PTSD. However, controlled studies have not been conducted to evaluate the safety or effectiveness of medical marijuana for PTSD. Thus, there is no evidence at this time that marijuana is an effective treatment for PTSD. In fact, research suggests that marijuana can be harmful to individuals with PTSD. [Boldness Added] Marijuana use has increased over the past decade. In 2013, a study found that 19.8 million people reported using marijuana in the past month, with 8.1 million using almost every day (1). Daily use has increased 60% in the prior decade (1). A number of factors are associated with increased risk of marijuana use, including diagnosis of PTSD (2), social anxiety disorder (3), other substance use, particularly during youth (4), and peer substance use (5). There has been no study of marijuana use in the overall Veteran population. What we do know comes from looking at data of Veterans using VA health care, who may not be representative of Veterans overall. When considering the subset of Veterans seen in VA health care with co-occurring PTSD and substance use disorders (SUD), cannabis use disorder has been the most diagnosed SUD since 2009. The percentage of Veterans in VA with PTSD and SUD who were diagnosed with cannabis use disorder increased from 13.0% in fiscal year (FY) 2002 to 22.7% in FY 2014. As of FY 2014, there are more than 40,000 Veterans with PTSD and SUD seen in VA diagnosed with cannabis use disorder (6). Marijuana use is associated with medical and psychiatric problems. These problems may be caused by using, but they also may reflect the characteristics of the people who use marijuana. Medical problems include chronic bronchitis, abnormal brain development among early adolescent initiators, and impairment in short-term memory, motor coordination and the ability to perform complex psychomotor tasks such as driving. Psychiatric problems include psychosis and impairment in cognitive ability. Quality of life can also be affected through poor life satisfaction, decreased educational attainment, and increased sexual risk-taking behavior (7). Chronic marijuana use also can lead to addiction, with an established and clinically significant withdrawal syndrome (8). Marijuana contains a variety of components (cannabinoids), most notably delta- 9-tetrahydrocannabinol (THC) the primary psychoactive compound in the marijuana plant. There are a number of other cannabinoids, such as cannabidiol (CBD), cannabinol (CBN), and cannabigerol (CBG). Marijuana can vary in cannabinoid concentration, such as in the ratio of THC to other cannabinoids (CBD in particular). Therefore, the effects of marijuana use (e.g., experience of a high, anxiety, sleep) vary as a function of the concentration of cannabinoids (e.g., THC/CBD). In addition, the potency of cannabinoids can vary. For example, the concentration of THC in the marijuana plant can range in strength from less than 1% to 30% based upon strain and cultivation methods. In general, the potency of THC in the marijuana plant has increased as much as 10-fold over the past 40 years (9,10). Recently, cannabis extract products, such as waxes and oils, have been produced and sold in which the concentration of THC can be as high as 90%. Thus, an individual could unknowingly consume a very high dose of THC in one administration, which increases the risk of an adverse reaction. Marijuana can be consumed in many different forms (e.g., flower, hash, oil, wax, food products, tinctures). Administration of these forms also can take different routes: inhalation (smoking or vaporizing), ingestion, and topical application. Given the same concentration/ratio of marijuana, smoking or vaporizing marijuana produces similar effects (11); however, ingesting the same dose results in a delayed onset and longer duration of effect (12). Not all marijuana users may be aware of the delayed effect caused by ingestion, which may result in greater consumption and a stronger effect than intended. Research has consistently demonstrated that the human endocannabinoid system plays a significant role in PTSD. People with PTSD have greater availability of cannabinoid type 1 (CB1) receptors as compared to trauma-exposed or healthy controls (13,14). As a result, marijuana use by individuals with PTSD may result in short-term reduction of PTSD symptoms. However, data suggest that continued use of marijuana among individuals with PTSD may lead to a number of negative consequences, including marijuana tolerance (via reductions in CB1 receptor density and/or efficiency) and addiction (15). Though recent work has shown that CB1 receptors may return after periods of marijuana abstinence (16), individuals with PTSD may have particular difficulty quitting (17). The belief that marijuana can be used to treat PTSD is limited to anecdotal reports from individuals with PTSD who say that the drug helps with their symptoms. There have been no randomized controlled trials, a necessary "gold standard" for determining efficacy. Administration of oral CBD has been shown to decrease anxiety in those with and without clinical anxiety (18). This work has led to the development and testing of CBD treatments for individuals with social anxiety (19), but not yet among individuals with PTSD. With respect to THC, one open trial of 10 participants with PTSD showed THC was safe and well tolerated and resulted in decreases in hyperarousal symptoms (20). People with PTSD have particular difficulty stopping their use of marijuana and responding to treatment for marijuana addiction. They have greater craving and withdrawal than those without PTSD (21), and greater likelihood of marijuana use during the six months following a quit attempt (17). However, these individuals can benefit from the many evidence-based treatments for marijuana addiction, including cognitive behavioral therapy, motivational enhancement, and contingency management (22). Thus, providers should still utilize these options to support reduction/abstinence. Treatment providers should not ignore marijuana use in their PTSD patients. The VA/DoD PTSD Clinical Practice Guideline (2010) recommends providing evidence-based treatments for the individual disorders concurrently. PTSD providers should offer education about problems associated with long-term marijuana use and make a referral to a substance use disorder (SUD) specialist if they do not feel they have expertise in treating substance use. Individuals with comorbid PTSD and SUD do not need to wait for a period of abstinence before addressing their PTSD. A growing number of studies demonstrate that that these patients can tolerate trauma-focused treatment and that these treatments do not worsen substance use outcomes. Therefore, providers have a range of options to help improve the lives of patients with the co-occurring disorders. For more information, see Treatment of Co-Occurring PTSD and Substance Use Disorder in VA. References Poster Comment: REPEAT: Marijuana Use and PTSD among Veterans
Epidemiology
Cannabis Use Disorder among Veterans Using VA Health Care
Problems Associated with Marijuana Use
Active Ingredients and Route of Administration
Neurobiology
Marijuana as a Treatment for PTSD
Treatment for Marijuana Addiction
Clinical Recommendations
Marijuana use for medical conditions is an issue of growing concern. Some Veterans use marijuana to relieve symptoms of PTSD and several states specifically approve the use of medical marijuana for PTSD. However, controlled studies have not been conducted to evaluate the safety or effectiveness of medical marijuana for PTSD. Thus, there is no evidence at this time that marijuana is an effective treatment for PTSD. In fact, research suggests that marijuana can be harmful to individuals with PTSD.
Post Comment Private Reply Ignore Thread
Top • Page Up • Full Thread • Page Down • Bottom/Latest
#1. To: Gatlin (#0)
Why do you hate veterans who have sought relief from PTSD? Veterans turn to forbidden cures for relief from their nightmares. For both men, the journey back to the land of the living began with illegal drugs. McCourry enrolled in a study of MDMA-assisted psychotherapy and was amazed by how quickly it made a difference. After years of insomnia and nightmares, he was suddenly able to sleep through the night. Within two years he felt like this "huge healing event had taken place," because he finally "had this sense of separation from the experiences of Marine combat." Pickering used marijuana to replace alcohol and the "kamikaze cocktail" of prescription drugs—sleeping pills, anti-anxiety meds, mood stabilizers—that had previously left him foggy. "It got my head back on straight," he says. "I still struggle sometimes, but I'm leaps and bounds beyond where I was." Isn't it nice to know that the VA isn't too busy deliberately putting vets on long waiting lists hoping for them to die that they can still find the money and the time to conduct a study about veteran's Reefer Madness?
I do not hat veterans who have sought relief from PTSD. I however do find despicable those deserving hatred and contempt who continually exploit and use veterans problems with PTSD to support their agenda for the unrestricted use of marijuana which is still on the Drug Enforcement Administration's list of scheduled drugs. Right at the very top, in fact.
Really? People have been praising the calming effect of marijuana for hundreds,maybe even thousands of years,and you yahoos can't find any evidence of it? It was even legal and sold by mail order right up to sometime in the 30's,when it was made illegal to protect the alcohol industry. IIRC,you could even buy it from a Sears catalog. HOW can something that had been noted for hundreds of years to reduce stress NOT be effective to treat Post Traumatic STRESS Syndrome? I KNOW the cops and the court systems are against legalization due to all the money and power they get from having it illegal,but aren't THEY supposed to have to answer to US? In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
You are an idiot. Do you believe EVERYTHING you read? In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
HOW can something that had been noted for hundreds of years to reduce stress NOT be effective to treat Post Traumatic STRESS Syndrome? Maybe it is because the medical controversy over whether marijuana helps veterans PTSD problems reveals a habit of human cognition in that simply thinking anecdotally is a natural reaction while thinking scientifically does not and requires intelligence. Agenda driven druggies more often accept anecdotal associations and make them so powerful that they want other people to ignore contrary evidence.
He probably has stock in big pharma. They hate anything that could help with disease if they don't make a profit from it. I do not go to church every time the doors are opened, but I love Jesus Christ. I am only human and fail Him daily. I believe Jesus is the Son of God, was born of a virgin, was crucified on a cross, died for my sins and rose from the dead and that He loves us dearly, and is faithful to forgive us of our sins. But He says that if you deny me in front of your friends I will deny you in front of my Father. Can I get an Amen!
I guess it depends on who is doing the control of the "controlled studies".
I do not go to church every time the doors are opened, but I love Jesus Christ. I am only human and fail Him daily. I believe Jesus is the Son of God, was born of a virgin, was crucified on a cross, died for my sins and rose from the dead and that He loves us dearly, and is faithful to forgive us of our sins. But He says that if you deny me in front of your friends I will deny you in front of my Father. Can I get an Amen!
I am not exploiting these veterans you obnoxious, self-righteous little prick, and neither are the doctors and researchers involved. They have chosen of their own free will to use a drug that has not been approved by fed.gov to help with their treatment for PTSD and other combat-related issues. Why? BECAUSE IT WORKS for them. If there any exploiting being done it is by you and the rest of the "Reefer Madness" cult who would stifle any research into the positive effects of cannabis and MDMA and force the veterans to use fed-approved drugs that have made their problems worse simply out of your cringing fear of something that you will never understand. That thought had occurred to me as well. That poster is known for his bragging about his portfolio. It seems likely that he has heavily invested in big pharma. I have a vietnam vet friend who was ecstatic a couple of years back when the VA shrinks finally took him off of prescription psych meds after decades of being on them. He just smokes marijuana occasionally now.
Get real …
Does it seem to help him ? Si vis pacem, para bellum Rebellion to tyrants is obedience to God. Never Pick A Fight With An Old Man He Will Just Shoot You He Can't Afford To Get Hurt "If there are no dogs in Heaven, then when I die I want to go where they went." (Will Rogers)
No one has done that. 25 Rules of Disinformation 7. Question motives. Twist or amplify any fact which could so taken to imply that the opponent operates out of a hidden personal agenda or other bias. Don't forget, it is the big pharma companies that are one of the leading opponents of marijuana legalization, along with alcohol companies, the prison industry and cops. Can't have something that will cut into that cash cow, right? Yes, he's much better off both physically and mentally, without the prescription crap.
You are an amazingly agenda driven biased individual, believing the anecdotal evidence of two individuals on marijuana and totally refusing to believe and fully reject the findings of two scientists who present a study showing contrary results. Your support in the use of anecdotes as evidence of causation commits a serious logical fallacy and means that anecdotal arguments must be rejected because they don’t give a fair representation. Anecdotes are worthless as evidence since they simply cannot demonstrate any casual relationships. For you to present a truly accurate picture, you need properly controlled studies that will accurately account for all confounding variables. Nothing else will suffice and unless proper scientific testing has shown causes, you are an idiot to conclude that there is a causal relationship between anything…..I don’t care how hard you continue to try and promote your druggie agenda. Give it up …
I dunno. Wasn't the guy who murdered Chris Kyle self-medicating with MJ? Maybe Doctor supervision might've helped in that case, or not.
Yeah - these are the only two who have benefited. Geesh, are you serious? By the way - here is one of YOUR beloved dealers of fed.gov approved drugs, the drugs you wish to see pushed to veterans and kids. No agenda here, right? Drug company founder John Kapoor arrested for alleged opioid scheme His company gave millions to fight marijuana legalization, and you think that's just swell. The Control-Freaks hate it when that happens.
You need to stay on point. The point is, you are supporting anecdotal evidence which is of course evidence based on personal experience. All you have are some brief narratives or stories that serve to make a point to further promote your agenda. You really should rely on empirical evidence that is based on scientific research. You fail to realize or will not acknowledge that the limitations of anecdotal evidence is that anecdotes are simply never factual. Although they make interesting reading, that doesn’t make them factual evidence. Why? Because they lack the time tested empirical evidence or facts and YOU need to be careful when making conclusions bases on anecdotal evidence and promoting it.
Yeah sure - I'm sure the soldiers just made up the story. Geesh!! There have been hundreds of similar examples of cannabis' effect on PTSD. Your problem is you don't want to see any scientific research done because - Reefer Madness. No - the point is, this is something that WORKS FOR THEM! It has worked for hundreds of other vets. You just don't like the fact that they are defying the government and choosing to use cannabis. You'd be happier if they were drugged to the gills with pharmacological prescription drugs instead. I like any well trained observer, Iong ago learned to view anecdotal evidence with the greatest amount of skepticism….if not outright disdain. It’s high time you also learn this. While anecdotal evidence is beguiling in its familiar involvement of our human sensibilities and responsibilities….it is however, as we all should learn, the enemy of an objective and dispassionate observation. Just because you read a personal story from someone that promotes your agenda in no way means that it is true. You must learn to use objectivity which means the state and high quality of being true even outside your strong individual biases and imaginings. Objectivity will set you free and make you a better person. This concludes my lesson for you today …
That is good. I am glad for him. I had three friends that suffered with PTSD. Not a good thing to have. Si vis pacem, para bellum Rebellion to tyrants is obedience to God. Never Pick A Fight With An Old Man He Will Just Shoot You He Can't Afford To Get Hurt "If there are no dogs in Heaven, then when I die I want to go where they went." (Will Rogers)
I have no agenda other than sanity and reason,and don't do drugs. I couldn't even smoke marijuana if it were legal because I have COPD and even have a hard time breathing though a surgical mask when I cut grass. People like you,on the other hand,have advanced cases of "Reefer Madness" and are afraid you would get high and sexually molest the family mule. In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
Depends who ya listen to, evidently. Routh's "heavy marijuana use" sure didn't seem to have a positive impact on Chris Kyle's health:
I seriously doubt he has stock in anything. I think his opinions are honest ones,even if wildly off-base. In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
You could do the edibles if you wanted to. Can you go anywhere in America and still find a "family mule"? Seems kinda dated. My grandfather had mules, liked them even. Because he was a very very tough old bastard. But he had teams of mules, not a "family mule". If you want to plow or pull old field implements, you need at least 2 mules if you're serious.
I had a little discussion about taking psych meds for PTSD with a doc at the VA maybe 30 years ago. First of all,I told him I did NOT have PTSD,didn't need his damn drugs because I already had all the confusion I needed trying to figure out the idiots in the civilian world,and that if they gave them to me I would throw them away. People are now drawing PTSD disability from the VA that have never been in a war or heard a shot fired. I worked with a guy in the post office that was receiving 30 or 40 percent disability (I forget which,now) for PTSD because he was stationed in Germany during the VN war as a telephone repairman/lineman,and lots of guys from his unit were getting transferred to VN. He told me himself that this worried him so much he had a nervous breakdown over it. PTSD was probably the best thing that ever happened to VA Hospital doctors,nurses,and administrators. Money FLOODED into the VA to treat "traumatic veterans",and the more the VA "found",the merrier. More shrinks were hired as well as support staff for them,and the VA budget just kept getting bigger and bigger. In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
Does it seem to help him ? If you had ever smoked pot,you would know that it's impossible to giggle at cartoons and be stressed at the same time. In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
From what I have seen,that is true for most mental patients. Don't get me wrong,there are clearly some people who are so confused on a permanent basis that the ONLY alternative to taking them out back and shooting them is to medicate them into oblivion to keep them from hurting themselves. Those psycho-active drugs are essential for these people because there is zero chance of any of them ever healing anyhow,so you sedate them. BYW,LSD was invented to help cure insane people,and then the bible thumpers and the other assorted moral midgets demanded it be outlawed "causen deys peepul out dare date eben habbin fun wid it!" Granted,there IS such a thing as too much of a good thing,but I personally know people who took LSD hundreds of times with no lasting apparent harm . Same thing with Magic Mushrooms and Peyote. Various Indian tribes used "magic mushrooms" for healing purposes. The feds tried to outlaw peyote too,but one western Indian Tribe was able to establish it was a part of their religious activities,so it was protected use under the Constitution. In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
You can't truly be THAT ignorant or gullible,can you? You are going to trust scientists on the government payroll that are paid to come to the "right" conclusion over the word of tens of thousands of people with personal experience? In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
He was/is a genuine nut case,and was most likely self-medicating with anything he could get his hands on,especially mental meds from the VA. In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
Of course the soldiers did not make up the story. They believe it and a strong belief is a practical instrument that can be used to shape reality. You do it every day….you decide what you believe. It is not the media or your friends….it is you. It is you who observes things and then decide what you BELIEVE. That, sport, is why belief creates facts to some. A pragmatist will always keep it real. If your mind can conceive it, you can believe it….that’s not an irresponsible quote.
Really? Watched hundreds of people smoking whacky-tabaccy and then took notes,did ya? Do tell all,please! In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
I don't know if they would work as well,and if I had it around,I'd be tempted to just smoke it. Can you go anywhere in America and still find a "family mule"? Sure,anywhere with people that think Reefer Madness is a documentary. In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
Depends who ya listen to, evidently. Routh's "heavy marijuana use" sure didn't seem to have a positive impact on Chris Kyle's health: Well,waddya expect to hear from two professional court witnesses,one paid by the prosecution to get a conviction,and the other paid by the defense to get a not guilty verdict? These people all have whatever opinion you want on anything,as long as you pay them. In the entire history of the world,the only nations that had to build walls to keep their own citizens from leaving were those with leftist governments.
LOL !!! Maybe he did, and that is why he is so adamant !!! ROFLMAO !!! Si vis pacem, para bellum Rebellion to tyrants is obedience to God. Never Pick A Fight With An Old Man He Will Just Shoot You He Can't Afford To Get Hurt "If there are no dogs in Heaven, then when I die I want to go where they went." (Will Rogers)
He was/is a genuine nut case Yeah, but opinions on how he became one are mixed: "substance-induced psychotic disorder," https://libertysflame.com/cgi-bin/readart.cgi? ArtNum=53281&Disp=26#C26 Likewise, the history, causation, and physiology of an individual's PTSD would vary. I always advise extreme caution to the veterans I encounter who are considering self-medicating with MJ -- especially those unfortunate souls who are under the VA's pharmacological "care". Those "medicines" and/or the withdrawal symptoms in the context of THC could produce results that are very dangerous for the individual and anyone in contact with them: Department of Veterans Affairs doctors are continuing to prescribe tranquilizers such as Valium and Xanax to veterans diagnosed with post- traumatic stress disorder — despite VA guidelines advising against their use for the condition. Almost a third of veterans being treated for PTSD are prescribed benzodiazepines, a class of sedatives commonly used to treat insomnia, anxiety, seizures and other conditions, according Dr. Nancy Bernardy, a clinical psychologist with the VA’s National Center for PTSD. https://www.stripes.com/news/sedatives-still- used-for-ptsd-treatment-despite-warnings-1.215000 "Using diazePAM together with cannabis (Schedule I substance) may increase side effects" https://www.drugs.com/drug-interactions/cannabis-with- valium-2758-0-862-441.html "Antipsychotics are generally ineffective for benzodiazepine withdrawal-related psychosis.[53][97] Antipsychotics should be avoided during benzodiazepine withdrawal as they tend to aggravate withdrawal symptoms, including convulsions.[28][98][99][100] Some antipsychotic agents may be more risky during withdrawal than others, especially clozapine, olanzapine or low potency phenothiazines (e.g., chlorpromazine), as they lower the seizure threshold and can worsen withdrawal effects; if used, extreme caution is required.[101] http s://en.wikipedia.org/wiki/Benzodiazepine_withdrawal_syndrome Etc. That's just one example.
Some Veterans use marijuana to relieve symptoms of PTSD and several states specifically approve the use of medical marijuana for PTSD. However, controlled studies have not been conducted to evaluate the safety or effectiveness of medical marijuana for PTSD. Thus, there is no evidence at this time that marijuana is an effective treatment for PTSD. In fact, research suggests that marijuana can be harmful to individuals with PTSD.
“Truth is treason in the empire of lies.” - Ron Paul

Those who most loudly denounce Fake News are typically those most aggressively disseminating it.
#2. To: Deckard (#1)
#3. To: Deckard (#1)
Why do you hate veterans who have sought relief from PTSD?
Veterans turn to forbidden cures for relief from their nightmares.

#4. To: Deckard (#1)
Thus, there is no evidence at this time that marijuana is an effective treatment for PTSD.
#5. To: Gatlin (#3)
I however do find despicable those deserving hatred and contempt who continually exploit and use veterans problems with PTSD to support their agenda for the unrestricted use of marijuana which is still on the Drug Enforcement Administration's list of scheduled drugs. Right at the very top, in fact.
#6. To: sneakypete (#5)
(Edited)
The reason for this cognitive disconnect is that we have evolved brains that pay attention to anecdotes because false positives (believing there is a connection between A and B when there is not) are usually harmless, whereas false negatives (believing there is no connection between A and B when there is) may take you out of the gene pool. Our brains are belief engines that employ association learning to seek and find patterns. Superstition and belief in magic are millions of years old, whereas science, with its methods of controlling for intervening variables to circumvent false positives, is only a few hundred years old. So it is that any medical huckster promising that A will cure B has only to advertise a handful of successful anecdotes in the form of testimonials.
#7. To: Deckard (#1)
Why do you hate veterans who have sought relief from PTSD?
#8. To: Deckard (#1)
(Edited)
#9. To: Gatlin (#3)
I however do find despicable those deserving hatred and contempt who continually exploit and use veterans problems with PTSD
“Truth is treason in the empire of lies.” - Ron Paul

Those who most loudly denounce Fake News are typically those most aggressively disseminating it.
#10. To: U don't know me (#7)
He probably has stock in big pharma.
“Truth is treason in the empire of lies.” - Ron Paul

Those who most loudly denounce Fake News are typically those most aggressively disseminating it.
#11. To: Deckard, Gatlin, sneakypete (#1)
Pickering used marijuana to replace alcohol and the "kamikaze cocktail" of prescription drugs—sleeping pills, anti-anxiety meds, mood stabilizers—that had previously left him foggy. "It got my head back on straight," he says. "I still struggle sometimes, but I'm leaps and bounds beyond where I was."
#12. To: U don't know me (#7)
He probably has stock in big pharma. They hate anything that could help with disease if they don't make a profit from it.
While those who blindly promote anecdotal associations for marijuana as a cure all for everything including PTSD have stock in marijuana production and distribution companies since those companies make a profit from marijuana….in fact marijuana sales totaled $6.7 billion in 2016.
#13. To: hondo68 (#11)
" I have a vietnam vet friend who was ecstatic a couple of years back when the VA shrinks finally took him off of prescription psych meds after decades of being on them. He just smokes marijuana occasionally now. "
#14. To: Gatlin (#12)
While those who blindly promote anecdotal associations for marijuana as a cure all for everything
“Truth is treason in the empire of lies.” - Ron Paul

Those who most loudly denounce Fake News are typically those most aggressively disseminating it.
#15. To: Stoner (#13)
Does it seem to help him ?
#16. To: Deckard (#14)
#17. To: Deckard (#1)
#18. To: Gatlin (#16)
(Edited)
You are an amazingly agenda driven biased individual, believing the anecdotal evidence of two individuals on marijuana
“Truth is treason in the empire of lies.” - Ron Paul

Those who most loudly denounce Fake News are typically those most aggressively disseminating it.
#19. To: Deckard (#9)
They have chosen of their own free will to use a drug that has not been approved by fed.gov to help with their treatment for PTSD and other combat-related issues. Why? BECAUSE IT WORKS for them.
#20. To: Deckard (#18)
(Edited)
#21. To: Gatlin (#20)
Although they make interesting reading, that doesn’t make them factual evidence.
“Truth is treason in the empire of lies.” - Ron Paul

Those who most loudly denounce Fake News are typically those most aggressively disseminating it.
#22. To: Gatlin (#20)
The point is, you are supporting anecdotal evidence which is of course evidence based on personal experience.
“Truth is treason in the empire of lies.” - Ron Paul

Those who most loudly denounce Fake News are typically those most aggressively disseminating it.
#23. To: Deckard (#22)
(Edited)
#24. To: hondo68 (#15)
" he's much better off both physically and mentally, without the prescription crap. "
#25. To: Gatlin (#6)
Agenda driven druggies more often accept anecdotal associations and make them so powerful that they want other people to ignore contrary evidence.
#26. To: Deckard (#21)
There have been hundreds of similar examples of cannabis' effect on PTSD. While Dr. Randall Price, a forensic psychologist who testified as the prosecution's medical expert, said Routh's heavy marijuana use caused a "substance-induced psychotic disorder," Dr. Mitchell Dunn said his opinion was that Routh's "psychosis was not substance-induced.""It is my opinion that he was suffering from a severe mental disease or defect that caused him not to know his conduct was wrong," Dunn testified.
#27. To: U don't know me (#7)
He probably has stock in big pharma.
#28. To: sneakypete (#25)
I have no agenda other than sanity and reason,and don't do drugs. I couldn't even smoke marijuana if it were legal because I have COPD and even have a hard time breathing though a surgical mask when I cut grass.
People like you,on the other hand,have advanced cases of "Reefer Madness" and are afraid you would get high and sexually molest the family mule.
#29. To: hondo68 (#11)
I have a vietnam vet friend who was ecstatic a couple of years back when the VA shrinks finally took him off of prescription psych meds after decades of being on them.
#30. To: Stoner (#13)
" I have a vietnam vet friend who was ecstatic a couple of years back when the VA shrinks finally took him off of prescription psych meds after decades of being on them. He just smokes marijuana occasionally now. "
#31. To: hondo68 (#15)
Yes, he's much better off both physically and mentally, without the prescription crap.
#32. To: Gatlin (#16)
You are an amazingly agenda driven biased individual, believing the anecdotal evidence of two individuals on marijuana and totally refusing to believe and fully reject the findings of two scientists who present a study showing contrary results.
#33. To: VxH (#17)
I dunno. Wasn't the guy who murdered Chris Kyle self-medicating with MJ?
#34. To: Deckard (#21)
Yeah sure - I'm sure the soldiers just made up the story. Geesh!!
There have been hundreds of similar examples of cannabis' effect on PTSD.
#35. To: Gatlin (#23)
I like any well trained observer,.....
#36. To: Tooconservative (#28)
(Edited)
You could do the edibles if you wanted to.
#37. To: VxH (#26)
#38. To: sneakypete (#25)
" afraid you would get high and sexually molest the family mule. "
#39. To: sneakypete (#33)
(Edited)
Sedatives still used for PTSD treatment despite warnings
Top • Page Up • Full Thread • Page Down • Bottom/Latest
[Home] [Headlines] [Latest Articles] [Latest Comments] [Post] [Mail] [Sign-in] [Setup] [Help] [Register]
