Health/Medical
See other Health/Medical Articles
Title: Marijuana Use and PTSD among Veterans
Source:
ptsd.va.gov
URL Source: https://www.ptsd.va.gov/professiona ... arijuana_use_ptsd_veterans.asp
Published: Oct 30, 2017
Author: Marcel O. Bonn-Miller, Ph.D. and Glenna
Post Date: 2017-10-30 08:11:42 by Gatlin
Keywords: None
Views: 6860
Comments: 39
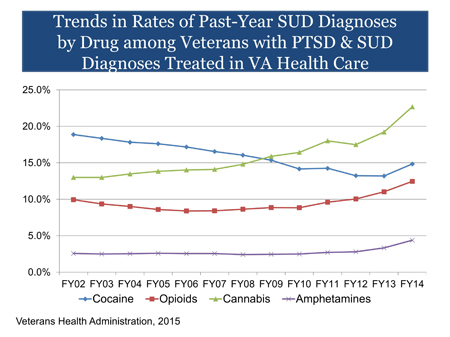
Marijuana use for medical conditions is an issue of growing concern. Some Veterans use marijuana to relieve symptoms of PTSD and several states specifically approve the use of medical marijuana for PTSD. However, controlled studies have not been conducted to evaluate the safety or effectiveness of medical marijuana for PTSD. Thus, there is no evidence at this time that marijuana is an effective treatment for PTSD. In fact, research suggests that marijuana can be harmful to individuals with PTSD. [Boldness Added] Marijuana use has increased over the past decade. In 2013, a study found that 19.8 million people reported using marijuana in the past month, with 8.1 million using almost every day (1). Daily use has increased 60% in the prior decade (1). A number of factors are associated with increased risk of marijuana use, including diagnosis of PTSD (2), social anxiety disorder (3), other substance use, particularly during youth (4), and peer substance use (5). There has been no study of marijuana use in the overall Veteran population. What we do know comes from looking at data of Veterans using VA health care, who may not be representative of Veterans overall. When considering the subset of Veterans seen in VA health care with co-occurring PTSD and substance use disorders (SUD), cannabis use disorder has been the most diagnosed SUD since 2009. The percentage of Veterans in VA with PTSD and SUD who were diagnosed with cannabis use disorder increased from 13.0% in fiscal year (FY) 2002 to 22.7% in FY 2014. As of FY 2014, there are more than 40,000 Veterans with PTSD and SUD seen in VA diagnosed with cannabis use disorder (6). Marijuana use is associated with medical and psychiatric problems. These problems may be caused by using, but they also may reflect the characteristics of the people who use marijuana. Medical problems include chronic bronchitis, abnormal brain development among early adolescent initiators, and impairment in short-term memory, motor coordination and the ability to perform complex psychomotor tasks such as driving. Psychiatric problems include psychosis and impairment in cognitive ability. Quality of life can also be affected through poor life satisfaction, decreased educational attainment, and increased sexual risk-taking behavior (7). Chronic marijuana use also can lead to addiction, with an established and clinically significant withdrawal syndrome (8). Marijuana contains a variety of components (cannabinoids), most notably delta- 9-tetrahydrocannabinol (THC) the primary psychoactive compound in the marijuana plant. There are a number of other cannabinoids, such as cannabidiol (CBD), cannabinol (CBN), and cannabigerol (CBG). Marijuana can vary in cannabinoid concentration, such as in the ratio of THC to other cannabinoids (CBD in particular). Therefore, the effects of marijuana use (e.g., experience of a high, anxiety, sleep) vary as a function of the concentration of cannabinoids (e.g., THC/CBD). In addition, the potency of cannabinoids can vary. For example, the concentration of THC in the marijuana plant can range in strength from less than 1% to 30% based upon strain and cultivation methods. In general, the potency of THC in the marijuana plant has increased as much as 10-fold over the past 40 years (9,10). Recently, cannabis extract products, such as waxes and oils, have been produced and sold in which the concentration of THC can be as high as 90%. Thus, an individual could unknowingly consume a very high dose of THC in one administration, which increases the risk of an adverse reaction. Marijuana can be consumed in many different forms (e.g., flower, hash, oil, wax, food products, tinctures). Administration of these forms also can take different routes: inhalation (smoking or vaporizing), ingestion, and topical application. Given the same concentration/ratio of marijuana, smoking or vaporizing marijuana produces similar effects (11); however, ingesting the same dose results in a delayed onset and longer duration of effect (12). Not all marijuana users may be aware of the delayed effect caused by ingestion, which may result in greater consumption and a stronger effect than intended. Research has consistently demonstrated that the human endocannabinoid system plays a significant role in PTSD. People with PTSD have greater availability of cannabinoid type 1 (CB1) receptors as compared to trauma-exposed or healthy controls (13,14). As a result, marijuana use by individuals with PTSD may result in short-term reduction of PTSD symptoms. However, data suggest that continued use of marijuana among individuals with PTSD may lead to a number of negative consequences, including marijuana tolerance (via reductions in CB1 receptor density and/or efficiency) and addiction (15). Though recent work has shown that CB1 receptors may return after periods of marijuana abstinence (16), individuals with PTSD may have particular difficulty quitting (17). The belief that marijuana can be used to treat PTSD is limited to anecdotal reports from individuals with PTSD who say that the drug helps with their symptoms. There have been no randomized controlled trials, a necessary "gold standard" for determining efficacy. Administration of oral CBD has been shown to decrease anxiety in those with and without clinical anxiety (18). This work has led to the development and testing of CBD treatments for individuals with social anxiety (19), but not yet among individuals with PTSD. With respect to THC, one open trial of 10 participants with PTSD showed THC was safe and well tolerated and resulted in decreases in hyperarousal symptoms (20). People with PTSD have particular difficulty stopping their use of marijuana and responding to treatment for marijuana addiction. They have greater craving and withdrawal than those without PTSD (21), and greater likelihood of marijuana use during the six months following a quit attempt (17). However, these individuals can benefit from the many evidence-based treatments for marijuana addiction, including cognitive behavioral therapy, motivational enhancement, and contingency management (22). Thus, providers should still utilize these options to support reduction/abstinence. Treatment providers should not ignore marijuana use in their PTSD patients. The VA/DoD PTSD Clinical Practice Guideline (2010) recommends providing evidence-based treatments for the individual disorders concurrently. PTSD providers should offer education about problems associated with long-term marijuana use and make a referral to a substance use disorder (SUD) specialist if they do not feel they have expertise in treating substance use. Individuals with comorbid PTSD and SUD do not need to wait for a period of abstinence before addressing their PTSD. A growing number of studies demonstrate that that these patients can tolerate trauma-focused treatment and that these treatments do not worsen substance use outcomes. Therefore, providers have a range of options to help improve the lives of patients with the co-occurring disorders. For more information, see Treatment of Co-Occurring PTSD and Substance Use Disorder in VA. References Poster Comment: REPEAT: Marijuana Use and PTSD among Veterans
Epidemiology
Cannabis Use Disorder among Veterans Using VA Health Care
Problems Associated with Marijuana Use
Active Ingredients and Route of Administration
Neurobiology
Marijuana as a Treatment for PTSD
Treatment for Marijuana Addiction
Clinical Recommendations
Marijuana use for medical conditions is an issue of growing concern. Some Veterans use marijuana to relieve symptoms of PTSD and several states specifically approve the use of medical marijuana for PTSD. However, controlled studies have not been conducted to evaluate the safety or effectiveness of medical marijuana for PTSD. Thus, there is no evidence at this time that marijuana is an effective treatment for PTSD. In fact, research suggests that marijuana can be harmful to individuals with PTSD.
Post Comment Private Reply Ignore Thread
Top • Page Up • Full Thread • Page Down • Bottom/Latest
Begin Trace Mode for Comment # 31.
#1. To: Gatlin (#0)
Why do you hate veterans who have sought relief from PTSD? Veterans turn to forbidden cures for relief from their nightmares. For both men, the journey back to the land of the living began with illegal drugs. McCourry enrolled in a study of MDMA-assisted psychotherapy and was amazed by how quickly it made a difference. After years of insomnia and nightmares, he was suddenly able to sleep through the night. Within two years he felt like this "huge healing event had taken place," because he finally "had this sense of separation from the experiences of Marine combat." Pickering used marijuana to replace alcohol and the "kamikaze cocktail" of prescription drugs—sleeping pills, anti-anxiety meds, mood stabilizers—that had previously left him foggy. "It got my head back on straight," he says. "I still struggle sometimes, but I'm leaps and bounds beyond where I was."
I have a vietnam vet friend who was ecstatic a couple of years back when the VA shrinks finally took him off of prescription psych meds after decades of being on them. He just smokes marijuana occasionally now.
Does it seem to help him ?
Yes, he's much better off both physically and mentally, without the prescription crap.
From what I have seen,that is true for most mental patients. Don't get me wrong,there are clearly some people who are so confused on a permanent basis that the ONLY alternative to taking them out back and shooting them is to medicate them into oblivion to keep them from hurting themselves. Those psycho-active drugs are essential for these people because there is zero chance of any of them ever healing anyhow,so you sedate them. BYW,LSD was invented to help cure insane people,and then the bible thumpers and the other assorted moral midgets demanded it be outlawed "causen deys peepul out dare date eben habbin fun wid it!" Granted,there IS such a thing as too much of a good thing,but I personally know people who took LSD hundreds of times with no lasting apparent harm . Same thing with Magic Mushrooms and Peyote. Various Indian tribes used "magic mushrooms" for healing purposes. The feds tried to outlaw peyote too,but one western Indian Tribe was able to establish it was a part of their religious activities,so it was protected use under the Constitution.
There are no replies to Comment # 31. End Trace Mode for Comment # 31.
Top • Page Up • Full Thread • Page Down • Bottom/LatestSome Veterans use marijuana to relieve symptoms of PTSD and several states specifically approve the use of medical marijuana for PTSD. However, controlled studies have not been conducted to evaluate the safety or effectiveness of medical marijuana for PTSD. Thus, there is no evidence at this time that marijuana is an effective treatment for PTSD. In fact, research suggests that marijuana can be harmful to individuals with PTSD.
#11. To: Deckard, Gatlin, sneakypete (#1)
Pickering used marijuana to replace alcohol and the "kamikaze cocktail" of prescription drugs—sleeping pills, anti-anxiety meds, mood stabilizers—that had previously left him foggy. "It got my head back on straight," he says. "I still struggle sometimes, but I'm leaps and bounds beyond where I was."
#13. To: hondo68 (#11)
" I have a vietnam vet friend who was ecstatic a couple of years back when the VA shrinks finally took him off of prescription psych meds after decades of being on them. He just smokes marijuana occasionally now. "
#15. To: Stoner (#13)
Does it seem to help him ?
#31. To: hondo68 (#15)
Yes, he's much better off both physically and mentally, without the prescription crap.
Replies to Comment # 31.
[Home] [Headlines] [Latest Articles] [Latest Comments] [Post] [Mail] [Sign-in] [Setup] [Help] [Register]
