Corrupt Government
See other Corrupt Government Articles
Title: Americans Who Opt Out of Medicare Must Forfeit Social Security Benefits
Source:
Breitbart
URL Source: http://www.breitbart.com/big-govern ... feit-social-security-benefits/
Published: May 31, 2016
Author: Dr. Susan Berry
Post Date: 2016-05-31 19:04:10 by cranky
Keywords: None
Views: 19790
Comments: 77
Most adults in the United States who turn 65 go onto the government-mandated health insurance program known as Medicare – the program liberal and socialist Democrats hope will universally cover all Americans some day soon. Seniors who choose to opt out of Medicare and continue to purchase their own private health insurance plans, however, are punished by the federal government for doing so by being forced to forfeit their Social Security benefits, even though they may have paid into the Social Security system for many years. Medicare and Social Security have been linked together since 1993 when unelected bureaucrats in the Clinton administration wrote a rule that states seniors cannot opt out of Medicare without giving up their Social Security benefits. In 2008, a group of seniors, who formed an organization called The Fund for Personal Liberty, filed a lawsuit – Hall v. Sebelius – in which they argued that the applications for Medicare and Social Security are voluntary and independent of each other. These Americans had all contributed to Medicare and Social Security throughout their employment histories, but wished to continue to purchase private health insurance once they reached age 65. They asserted that they should be able to opt out of Medicare – government-run healthcare – without forfeiting their Social Security benefits, and that forced participation in Medicare violates the right to privacy. The Fund wrote: The Medicare Lawsuit challenges the idea that unelected bureaucrats can create policies that act as law. Nowhere in the Medicare and Social Security statutes will you find a provision that a person who wishes to avoid Medicare shall be denied Social Security benefits. That is a penalty of approximately $250,000. The case proceeded for several years and hit its most alarming obstacle in March of 2011, when U.S. District Judge Rosemary Collyer – former general counsel of the National Labor Relations Board – who initially had sided with the plaintiffs, suddenly reversed herself, ruling in favor of the Obama administration instead. In an earlier ruling in the case, Collyer acknowledged that, “neither the statute nor the regulation specifies that Plaintiffs must withdraw from Social Security and repay retirement benefits in order to withdraw from Medicare.” In her stunning reversal decision, however, the judge ruled that “requiring a mechanism for plaintiffs and others in their situation to ‘dis-enroll’ would be contrary to congressional intent, which was to provide ‘mandatory’ benefits under Medicare Part A and for those receiving Social Security Retirement benefits.” Collyer also asserted in her decision that the Obama administration “extols the benefits of Medicare Part A and suggests that Plaintiffs would agree they are not truly injured if they were to learn more about Medicare, perhaps through discovery.” “Plaintiffs are trapped in a government program intended for their benefit,” she continued. “They disagree and wish to escape. The Court can find no loophole or requirement that the Secretary provide such a pathway.” Regarding the decision, Kent Masterson Brown, the lead attorney representing the seniors in the case, commented at the time: Anyone concerned with what will happen when the bureaucrats start writing the thousands of pages of rules that will govern the ‘Patient Protection and Affordable Care Act’ need only look at what has happened in Hall v. Sebelius. When they do, they will realize nothing will be optional and there will be no fair, affordable or swift manner to obtain recourse or appeal a decision made by the bureaucracy. After the ruling, which essentially decided that an entitlement program such as Medicare is “mandatory,” then-Sen. Jim DeMint (R-SC) introduced the Retirement Freedom Act. The bill would have allowed Medicare and Social Security to be “disconnected,” so that Americans would be free to opt out of government Medicare health insurance, but still retain their Social Security benefits. The bill, nevertheless, died in the Senate. Meanwhile, the members of the Fund appealed their case to the U.S. Supreme Court. In 2012, the Cato Institute and the American Civil Rights Union (ACRU) joined the case as well and submitted amicus briefs. However, in January of 2013, the Supreme Court denied the appeal, a decision the Fund stated was “the easy way out.” “The three branches of government all have the ability to reign in bureaucratic overreach, but none have the fortitude to do so,” wrote the Fund. “When unelected bureaucrats create mandates out of thin air, without any repercussions, we have opened Pandora’s Box.” 
Unelected bureaucrats recently proposed the imposition of a new rule that would affect all Medicare Part B providers and nearly all Medicare drugs. Such bureaucrats, however, have been operating for years, forcing Americans onto government-run healthcare under pain of loss of Social Security benefits.
(1 image)
Post Comment Private Reply Ignore Thread
Top • Page Up • Full Thread • Page Down • Bottom/Latest
Comments (1-37) not displayed.
.
.
.
#38. To: SOSO (#37)
The limits were on what the doctors could charge. The plaintiff's, by law, could only be charged LESS, and Uncle Sugar picked up most of the bill. The Secondary Insurer picked up all, or virtually all, the rest. Medicare eliminates the deductible for a doctor's visit. Please quit the obscene bullshit. I have explained it to you nine ways to Sunday. See #14: We conclude that Armey and Hall have suffered injuries in fact from their reduced private insurance. See SOSO #16, in which you are caught pulling your response out of your ass. [SOSO #16] [SOSO] Total BS. Courts have the duty to determine what allegations have merit and what do not. Otherwise again BS allegation must be accepts for the purpose of standing. The court is not bound to accept every allegation for the purposes of standing. [nolu chan #35] "For purposes of ruling on a motion to dismiss for want of standing, both the trial and reviewing courts must accept as true all material allegations of the complaint, and must construe the complaint in favor of the complaining party." E.g., Jenkins v. McKeithen, 395 U. S. 411, 395 U. S. 421-422 (1969). You continually misrepresent what was said as a holding of the court. It was a review of an inquiry on standing where the court must accept the allegations as true, in order to determine whether the complainant has alleged facts, which if true, would justify proceeding to trial on the merits. In the proceedings on the merits, those allegations still need to be proven. On the merits, the case failed. The case was lost. Deal with it.
Exactly. That is why some of the better docs decide not to accept medicare. And that is why only the wealthy get care from those better docs. I guess you do not think that a person is injured when they no longer can get treatment from a better doctor because the government forced them to have to pay more because their existing private insurer no longer covered what that doctor was charging. NB - The private insurance company very likely negotiated a payment arrangement with that specific provider which undoubtedly was lower than the doctor's posted rated to the uber cash paying rich, such as the Kennedys. Now I agree that the billing practices of doctors and hospitals are a sham. The face value of the services provided to my wife (i.e. - what was billed to the insurance company) for treatment of her brain cancer, from surgery through the present clinical trial, is well in excess of $400,000. After the "discounts" negotiated by my private insurer, the actual payment was less than 30 cents on the dollar and my annual out of pocket cash expense was capped at well less than $8,000. Even though we had Medicare A it was not in the picture because is was still worker and my private insurance was primary at the time of her hospitalization. I just retired and Medicare A is now my primary for hospitalization and our private insurance secondary. I have not enrolled in Medicare B so my private insurance is still primary for these service. We are hoping that my wife will not need another surgery but if she does I am not at all sure that the combination of Medicare A as primary and my private insurance now as secondary will cover all of the cost ex. my stated annual out of pocket expense. I am trying to figure out what would happen if we did enroll in Medicare B. It is not at all clear that I would be at least as well covered as when I was not retired. Somehow I feel that we would be screwed. потому что Бог хочет это тот путь
No, you know that is bass ackwards as the Court stated. plaintiffs contend that entitlement to Medicare Part A benefits has thereby been made a prerequisite to receiving Social Security benefits, in contravention of the statute governing entitlement to Social Security benefits. But plaintiffs have it backwards. Signing up for Social Security is a prerequisite to Medicare Part A benefits, not the other way around. SS is in no way tied to obtainment, signing up for, or eligibility for Medicare. Cite the law or regulation that says it is. SOSO #7: "You need to do more research. Bill Clinton signed the operative law. " SOSO #9: [Quoting a blogger] "While the Social Security law does not require participants to accept Medicare, and the Medicare law does not require participants to accept Social Security, the Clinton Administration in 1993 tied the programs together. Under that policy, any senior who withdraws from Medicare also loses Social Security benefits." SOSO #12: "But it [a link] seems to be there between SS and Medicare A." SOSO #17: "HINT: It's so because the courts say it is so because that is the intent of Congress that made the law and Clinton who signed it." SOSO #32: "The fact is Congress tied SS to Medicare when it made the law that one could not refuse Medicare A and maintain their SS. You have repeatedly talked about this unidentified law alleged signed by Bill Clinton. Put up or shut up. Identify the law. I have linked and posted actual law. Where's yours??? What is your phantom law? What is it? What does it say? xx U.S.C. xxxx
I have not enrolled in Part B as my private insurance pays for it. The cost of my private insurance would not be reduced by my paying to have the government cover the cost. I believe BCBS is better and the govt won't screw with that because all the congressmen use it. As for the lawsuit, you can construe it any which way you want, but the requested remedy was contrary to statute law and the Court was legally barred from providing it. The statement that they were harmed was made assuming their allegations were true, and construing all doubts in favor of the plaintiff. There is no viable claim against Medicare as the law is clear and specific. Any remedy would have to come from Congress, not the Court. As for docs who do not participate in Medicare (not a penny acceptance of Medicare funds) you should be able to use your private insurer or money. In general, those providers would be expensive.
You missed the whole point of this thread. Upon retirement you automatically become eligible for Medicare A. As a result your private insurance only covers the amount that is determined by Medicare A, even though the day before it was covering a higher amount for you when you were not eligible for Medicare A. You lose coverage. You have to pay more out of pocket. The same is true for what your private insurance will pay to providers that do not accept Medicare. i.e. - it is my understanding that when Medicare is primary by law the insurance company can only pay the Medicare determined amount for a particular service (which may very well be lower than what it was paying the same provider when Medicare was not primary). If you were already collecting Social Security retirement benefits when you turned 65, you will automatically be enrolled Medicare Part A irrespective of whether or not you have private insurance. Prior to retirement your private insurance is primary and Medicare A secondary. The amount paid to providers is almost always negotiated between the provider and the insurance company - and it is usually above what Medicare A will pay. When you retire Medicare becomes primary. At that time if your private insurance reduces what it pays for a service to what is allowed by Medicare A you are injured just by the fact that Medicare A is considered primary. This judge ruled that the law is that one cannot reject Medicare eligibility. I am not quibbling with that finding but am outraged with the law. As for Medicare B vs. BCBS when you retire, I have no idea if you would be better off with just BCBS, with just Medicare B or paying for both. As you noted, most private insurance will cover the deductibles and copays under Medicare. This could be more than the premium paid for the BCBS coverage. To the extent that BCBS pays for services not covered by Medicare B you easily could be ahead of the game by have both coverages. This is what I am trying to determine with respect to my private insurance now that I am retired. When all is said and done tying Medicare to SS and not allowing a person to be free of Medicare eligibility just screws most retirees by providing a lower level of service or by forcing them to pay more for the same level of coverage. On last time, do you think this is what the Founding fathers intended? потому что Бог хочет это тот путь
No, Medicare becomes your primary insurer and pays most of the cost and yor private insurer become secondary and pays the remainder. You pay little to nothing out of pocket.
Thank you for posting this case, nolo chan. As always, I enjoy reading your posts even if we disagree. I love conversing with intelligent people like yourself.
Only up to the amount established by Medicare which I believe is less than what the private insurers pay when they are primary. The net result is that your out of pocket expense increases. потому что Бог хочет это тот путь
The only duty the Courts have is to determine three things: 1)personal jurisdiction over you, jurisdiction to hear your case, and finally standing to sue not just based on the merits of your case alone. There could be substantive laws of procedure that would compel such a panel of judges to grant review of your case. This may be referred to as Judicial Review possibly by a panel of judges at an en banc hearing.
As this case reads standing was determined on the basis of whether the plantiffs were injured. RE: post #14: "They claim they would receive enhanced coverage from their private insurers if they were not entitled to Medicare Part A benefits. For purposes of the standing inquiry, we must accept those declarations as true. We conclude that Armey and Hall have suffered injuries in fact from their reduced private insurance. They have shown causation because their private insurance has been curtailed as a direct result of their legal entitlement to Medicare Part A benefits. And as to redressability, plaintiffs claim that they could obtain additional coverage from their private insurance plans if allowed to disclaim their legal entitlement to Medicare Part A benefits. Because Armey and Hall have standing, we need not address standing for the other plaintiffs. We therefore proceed to the merits." Is there any way to read those paragraphs that leads to the conclusion that the judge found that the plantiffs were in fact injured, that the basis for establishing plantiifs standing was that injury, and, that the merits of the case were something other than that injury? потому что Бог хочет это тот путь
Is there any way to read those paragraphs that leads to the conclusion that the judge found that the plantiffs were in fact injured, That would have to be determined by the causation leading to the injury. ... that the basis for establishing plantiifs [sic] standing was that injury, Again, that would be determined by the causation stated in Plaintiff's Complaint concerning that injury. You might want to re-read post 11. Cause this is what I got from it. II We first consider plaintiffs' standing. Plaintiffs claim that their private insurers have curtailed coverage as a result of plaintiffs' entitlement to Medicare Part A benefits. Plaintiff Armey declared that his legal entitlement to Medicare Part A benefits led his Blue Cross plan to reduce coverage without a matching reduction in premium. Plaintiff Hall declared that his Mail Handlers plan stopped acting as his primary payer because of his legal entitlement to Medicare Part A benefits. They claim they would receive enhanced coverage from their private insurers if they were not entitled to Medicare Part A benefits. For purposes of the standing inquiry, we must accept those declarations as true. [Emphasis added here]
That doesn't square with your post #46. потому что Бог хочет это тот путь
Actually it does. The reason why is that the judges in this matter relied on the Plaintiff's sworn Declarations that were attached to the Verified Complaints. Not excluding the federal statutes on rules of civil procedures on merits of cases, Declarations are used as part of the Complaint and although they are not incorporated into each paragraph, the Declaration (or sworn Affidavit) as separate from the Complaint, is just as important as the Complaint and stated causes of actions incorporated into each paragraph itself.
Negative. The amount the provider can charge decreases to what Medicare allows. I will provide my personal info from April. The figures come straight off my BCBS paperwork. An MRI had charges submitted by the imaging center for $2,214.00. The Medicare Plan Allowance was $245.51. Medicare paid $148.77. BCBS paid the remainder $96.74. I paid nothing. Absent Medicare, the bill would have been $2,214.00. Had a private insurer paid 90% (no deductible), that would have left a bill of $221.40. When the provider participates in Medicare, they agree to accept the plan allowance as full payment, in this case $245.51. If I had no secondary insurer, I could have been billed not more than $96.74 out of pocket. Because Medicare lowballs the plan allowance so much, the providers increase what they charge others so they can remain profitable. It is not the Medicare patient whose out of pocket expenses increase, it is the non-Medicare expenses that increase.
Where did you get an MRI billed for only $2,214? потому что Бог хочет это тот путь
So you are claiming that the plantiffs lied about having to pay more when Medicare became primary? потому что Бог хочет это тот путь
Were they required to do that as they stated that they must or did they just accept the plantiffs declarations without further inquiry? потому что Бог хочет это тот путь
And that's exactly the catch. If my provider of choice does not accept Medicare but had a separate agreement with the insurance company the insurance company would in almost all cases pay more for that provider's service than the Medicare amount. When I then become locked into mandated Medicare the insurance company automatically reduces what it will pay my provider of choice for a particular service. So when I now again go to my provider of choice I will have to pay more out of pocket if I want treatment by that provider. My alternative is to find another provider that accepts Medicare. It's Obama's lie again, "if you want to keep your provider you can......but it may very well cost you." No matter how you cut it Big Brother is forcing us to take Medicare whether we like it or not. Only the wealthy (including the lawmakers) will be able to afford the provider of their choice and there will only be room for a few them. Again I ask you, is this what you believe that the Founding Fathers intended? потому что Бог хочет это тот путь
OK, your provider accepts Medicare. When my wife was diagnosed with brain cancer we chose our providers on the basis of skill, reputation, recommendations from people in the medical community, etc. AND if they were covered by our private insurance which at the time was primary (though we had Medicare A no Medicare was involved as I still was working). Medicare did not come into our thinking at the time we chose our providers. Frankly I have no idea if our providers accept Medicare or not. If they do our experience going forward with her treatments may likely follow yours. If not we will likely have to pay significantly more out of pocket OR change providers in mid-stream of long-term treatment. If the latter we will certainly feel that we lost something as we chose our providers very carefully from among of several alternatives - obviously we felt we chose the best providers available to us at the time. Medicare did not enter into the picture. Enter Medicare and we may now have to choose what we view as lesser skilled providers and/or facilities. And the picture is even more uncertain as we are almost certain to have to find another clinical trial in the not too distant future with Medicare A now our primary insurance. We have been in contact with a few of the most notable doctors in the country to establish a relationship with them when the time comes for us to move on. I have no idea if these most prominent neuro- oncologists and neuro-surgeons accept Medicare. If they don't I don't know if we will be able to afford the treatment. I do know for a fact that Ted Kennedy had no money problems with being able to engage one or more of these doctors to treat his brain cancer. Dealing with incurable cancer is scary enough not to have to worry about losing some insurance coverage because of a government mandate. потому что Бог хочет это тот путь
Baptist.
No, I am saying you are mistaken about what plaintiffs claimed.
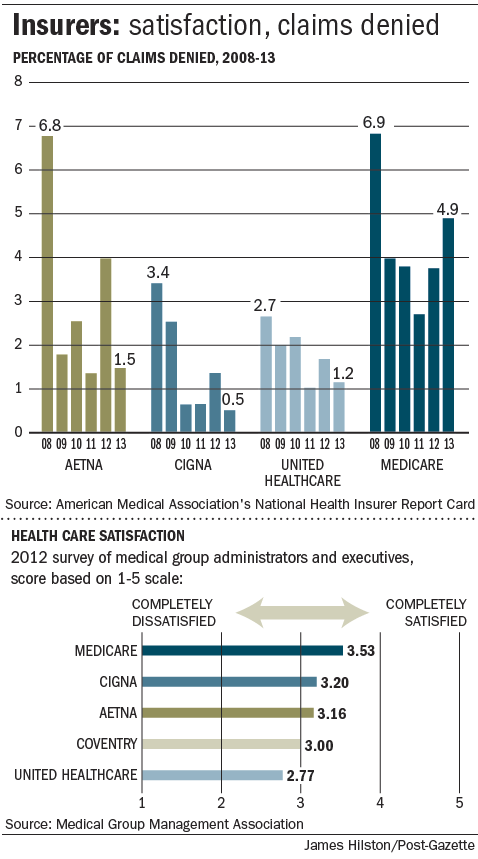
With its higher denial rate please tell me again why mandated Medicare does not represent a lowering of medical care for patients. "In its most recent report from 2013, the association found Medicare most frequently denied claims, at 4.92 percent of the time; followed by Aetna, with a denial rate of 1.5 percent; United Healthcare, 1.18 percent; and Cigna, 0.54 percent.' When Medicare is primary and private insurance secondary, what do the private insurers cover when Medicare denies a claim? потому что Бог хочет это тот путь
OK, please tell me what injury did they claim? потому что Бог хочет это тот путь
When you are 65 and eligible for Social Security, you automatically become entitled to Medicare Part A. The vast majority of people over 65 are eligible for Social Security and have Medicare Part A bestowed upon them. If you choose not to accept Medicare Part A benefits, that's your choice. It will cost you a small fortune to use an opt-out provider. You should find out for absolute certain what your private insurer would pay. A mistake could be very, very expensive. In general, if you see an opt-out provider, you must enter into a contract for his services and you are responsible for the full payment. In general, when you become entitled to Medicare Part A, the private insurer diminishes their responsibility to pay. They do not volunteer to pick up a $2K tab for a procedure for which 99% of providers will accept about $250. Entitlement has been automatic since Lyndon Johnson signed it into law. Obama hadn't turned 4 years old yet. About 99% of providers accept Medicare. You are not forced to take Medicare benefits, but you are automatically entitled to the benefits. Your for-profit insurance company acts accordingly. It depends. Some wanted a monarchy. Some immediately went about the business of interpreting and transforming the Constitution. Within a few years, America had the Alien and Sedition Acts. The transformation did not happen by accident.
There is a Wikipedia article on the case: https://en.wikipedia.org/wiki/Hall_v._Sebelius This case was before the court multiple times. A review may (or may not) clarify the various characterizations of the specific complaint, and the DHHS failed motion for dismissal based on asserted lack of standing. HALL v. SEBELIUS, 689 F. Supp.2d 10 (D.D.C. 2009) Brian Hall, Lewis Randall, Norman Rogers, John J. Kraus, and Richard K. Armey are retirees who "do not want to apply for, or want to disenroll from Medicare, Parts A and B . . . [but] do want to apply for and/or be paid their monthly Social Security benefits to which they are entitled." Am. Compl. [Dkt. # 4] ¶ 11. They have filed this lawsuit pursuant to the Medicare Act, 42 U.S.C. § 1395 et seq., the Social Security Act, 42 U.S.C. § 401 et seq., and the Administrative Procedure Act ("APA"), 5 U.S.C. § 551 et seq., alleging that the Social Security Administration's ("SSA") regulations regarding Medicare Part A, as set forth in the SSA's Program Operations Manual System ("POMS") are invalid and operate either to deprive Plaintiffs of their right to Social Security benefits or to force them to "enroll in" Medicare Part A against their will. Defendants Kathleen Sebelius, Secretary of the Department of Health and Human Services ("HHS") — of which the SSA is a part — and Michael J. Astrue, Commissioner of the SSA, move to dismiss. Dkt. # 12. Randall and Rogers were dropped due to lack of standing. The DHHS motion to dismiss was denied and the case with three plaintiffs continued to District Court where the Court granted summary judgment for DHHS. HALL v. SEBELIUS, 770 F. Supp.2d 61 (D.D.C. 2011) ROSEMARY M. COLLYER, District Judge. Plaintiffs are retired Federal employees who have reached age 65 and have applied for, and are receiving, Social Security Retirement benefits. As a result, they are "entitled" to Medicare Part A, coverage. They do not, however, want Medicare coverage. And the only avenue provided to Plaintiffs to un-entitle themselves is to cease receiving Social Security Retirement benefits — and to repay all such benefits already received. Plaintiffs declaim that such a requirement is contrary to the Social Security Act, of which Medicare is a part. The Court concludes that Plaintiffs' claims are without merit. Medicare costs are skyrocketing and may bankrupt us all; nonetheless, participation in Medicare Part A (for hospital insurance) is statutorily mandated for retirees who are 65 years old or older and are receiving Social Security Retirement (so-called 'old age') benefits. Whether Congress intended this result in 1965 or whether it is good fiscal and public policy in 2011 cannot gainsay the language of the statute and the regulations. Accordingly, summary judgment will be entered for Defendants. [...] III. ANALYSIS While the Court finds that Plaintiffs have standing with which to bring this lawsuit, they cannot survive summary judgment because the statutory scheme dictates that Medicare Part A is mandatory for those individuals who are 65 years old and are receiving Social Security Retirement benefits. A. Standing Exists Messrs. Kraus, Armey, and Hall have applied for and are receiving monthly Social Security Retirement benefits and wish to continue to do so; however, they wish to opt-out of Medicare Part A for various personal, financial, and other reasons. Defendants argue Plaintiffs have no standing to sue. As the Court found in Iyengar v. Barnhart, [I]n order [] for plaintiffs to establish their standing to sue, they need not eliminate all doubt as to whether the challenged action . . . caused [their injury]. . . . Rather, plaintiffs must show only (1) a substantial probability that [their injury] was or is being caused by the [defendant's] policy, and (2) a reasonable likelihood that eliminating that policy will [redress that injury]. 233 F. Supp. 2d 5, 10 (D.D.C. 2002). Plaintiffs' alleged injury is being forced to either (1) have inferior insurance foisted upon them, thereby precluding their ability to be covered by superior insurance; or (2) receive their superior non-Medicare Part A insurance at the cost of relinquishing their Social Security Retirement benefits, and re-paying past benefits received. Plaintiffs ask the Court to remedy this injury by invalidating the internal regulations that dictate this untenable choice — internal regulations which Plaintiffs claim are in contravention of the Social Security Act and the Medicare Act. Assuming this to be the case, the Court would have the power to invalidate those contravening regulations, thereby providing Plaintiffs with the redress they request. The Secretary extolls the benefits of Medicare Part A and suggests that Plaintiffs would agree they are not truly injured if they were to learn more about Medicare, perhaps through discovery. See, e.g., Defs.' Statement of Genuine Issues of Material Fact with Respect to Pls.' Mot. for Summ. J. [Dkt. #41] ¶ 35. Plaintiffs politely decline. The parties use a lot of ink disputing whether Plaintiffs' desire to avoid Medicare Part A is sensible. This is not an issue the Court needs to address. Plaintiffs have standing because they cannot avoid Medicare without forgoing Social Security Retirement benefits; they argue that there is no statutory tie between the two. This dispute constitutes a case or controversy without regard to why Plaintiffs prefer other insurance coverage. As such, Plaintiffs have standing to bring this lawsuit. [...] V. CONCLUSION Plaintiffs are trapped in a government program intended for their benefit. They disagree and wish to escape. The Court can find no loophole or requirement that the Secretary provide such a pathway. Defendants' Motion for Summary Judgment [Dkt. # 42], which was previously denied without prejudice, is reconsidered and will be granted and Plaintiffs' Motion for Summary Judgment [Dkt. # 51] will be denied. A memorializing Order accompanies this Memorandum Opinion. And the case made it to Circuit Court where the appeal failed: Hall v. Sebelius, No. 11-5076 (D.C. Cir. May 30, 2012) We first consider plaintiffs' standing. Plaintiffs claim that their private insurers have curtailed coverage as a result of plaintiffs' entitlement to Medicare Part A benefits. Plaintiff Armey declared that his legal entitlement to Medicare Part A benefits led his Blue Cross plan to reduce coverage without a matching reduction in premium. Plaintiff Hall declared that his Mail Handlers plan stopped acting as his primary payer because of his legal entitlement to Medicare Part A benefits. They claim they would receive enhanced coverage from their private insurers if they were not entitled to Medicare Part A benefits. For purposes of the standing inquiry, we must accept those declarations as true. We conclude that Armey and Hall have suffered injuries in fact from their reduced private insurance. They have shown causation because their private insurance has been curtailed as a direct result of their legal entitlement to Medicare Part A benefits. And as to redressability, plaintiffs claim that they could obtain additional coverage from their private insurance plans if allowed to disclaim their legal entitlement to Medicare Part A benefits. Because Armey and Hall have standing, we need not address standing for the other plaintiffs. We therefore proceed to the merits. [...] III Because plaintiffs are 65 or older and are entitled to Social Security benefits, they are "entitled to hospital insurance benefits" through Medicare Part A. 42 U.S.C. § 426(a). But plaintiffs do not want to be legally entitled to Medicare Part A benefits. What plaintiffs really seem to want is for the Government and, more importantly, their private insurers to treat plaintiffs' decision not to accept Medicare Part A benefits as meaning plaintiffs are also not legally entitled to Medicare Part A benefits. But the problem is that, under the law, plaintiffs remain legally entitled to the benefits regardless of whether they accept them. And a petition for rehearing was denied: Hall v. Sebelius, 667 F.3d 1293 (D.C. Cir. 2012) Upon consideration of appellants' petition for panel rehearing filed on March 22, 2012, and the response thereto, it is ORDERED that the petition be denied. [...] HENDERSON, Circuit Judge, specially concurring: My colleague concurring in the denial of panel rehearing is apparently surprised that the "[p]laintiffs' petition for rehearing appears to reflect some misunderstanding about our holding in this case." Concurrence at 3 (Kavanaugh, J.). I, in contrast, am in no way surprised by the substance of the plaintiffs' petition, especially its assertion that the majority's holding "is over an issue that was not even before the Court." Pl.'s Pet. 1. Any disconnect between the panel majority opinion and the plaintiffs' petition is the consequence of the opinion's own avoidance of the sole issue in this case: Whether the Social Security Administration is authorized to penalize an individual who declines Medicare, Part A coverage by requiring him to forfeit his Social Security retirement benefits and repay any benefits previously received. The plaintiffs pushed the issue in their opening brief, see, e.g., Appellant's Br. 22 ("The POMS require, subject to severe penalty for non-compliance, what Congress made to be purely voluntary."), and again in their reply brief, see, e.g., Appellant's Reply Br. 4 ("The only issue is whether 'entitlement' under § 426(a) means that a person so entitled must accept Medicare, Part A, benefits as a condition of receiving Social Security retirement benefits."). Like a parent who yells "get in the game" to his child picking daisies in the outfield, the plaintiffs ask the court to "get in the game" and finally address the issue it ignored. See Pl.'s Pet. at 4-5 ("[T]he actual question placed before this Court is whether the Social Security Administration can lawfully promulgate a quasi-regulatory provision that penalizes individuals who seek to decline coverage under Medicare, Part A, by requiring them to forfeit their Social Security retirement benefits."). While I consider the plaintiffs' rehearing petition to be an exercise in futility and therefore do not dissent from the denial thereof, I feel compelled to point out my concurring colleague's insistence on miscalling the game. KAVANAUGH, Circuit Judge, with whom Senior Circuit Judge Ginsburg joins, concurring in the denial of panel rehearing: Plaintiffs' petition for rehearing appears to reflect some misunderstanding about our holding in this case. To be crystal clear, no one is forced to accept Medicare Part A benefits for hospitalization costs. Someone who is 65 or older and has signed up for Social Security is automatically entitled to Medicare Part A benefits. But that person is not forced to accept those Medicare benefits. What really seems to be going on in this case is that plaintiffs' private insurers are curtailing coverage because plaintiffs have another source of coverage - namely, Medicare Part A. Plaintiffs are not happy that their private insurers are in effect penalizing them based on their entitlement to Medicare Part A benefits. Plaintiffs therefore want to "disenroll" from Medicare Part A. They claim a statutory right to "disenroll" and argue that the Department of Health and Human Services and the Social Security Administration have improperly denied them that right. No matter how plaintiffs label it, however, their grievance about the private insurance consequences of their entitlement to Medicare Part A benefits would be answered only if (i) the private insurers did not penalize plaintiffs based on their entitlement to Medicare Part A benefits or (ii) plaintiffs could somehow disclaim their entitlement to Medicare Part A benefits in a manner that would satisfy the private insurers that plaintiffs are not entitled to another source of coverage. We obviously cannot do anything here about the coverage practices of private insurers. And the statute simply provides no mechanism for a person who is 65 or older and has signed up for Social Security to disclaim his or her entitlement to Medicare Part A benefits (or to "disenroll," as plaintiffs put it). To reiterate, no one is forced to take Medicare Part A benefits. But the key problem for plaintiffs is that their private insurers apparently will not ignore the fact that plaintiffs are able to obtain Medicare Part A benefits. One of the consequences of the expanded social safety net fashioned by the Federal Government is that private entities or charities sometimes adjust benefits based on whether a recipient is otherwise entitled to government-provided benefits. We recognize that plaintiffs are frustrated with this particular manifestation of that broader phenomenon. But absent a constitutional or statutory violation, it is not our role to police that allocation of government and private resources.
Nothing. The claim was denied. Nobody, including the patient, is paying anything for it.
The COMPLAINT in Hall v. Sebelius was filed in the District Court. The Opinion we have been discussing is from the Circuit Court of Appeals.
It took you a while but thanks for seeing the light. Yes, if my current providers of choice do not accept Medicare then we will be injured in one of two ways or perhaps both. First, if I chose to continue with THE PROVIDER OF MY CHOICE WHICH I HAD BEFORE MEDICARE WAS FORCED UPON ME I will have to pay more, perhaps more than I can afford OR I will have to chose a provider of lesser quality as we judge that. The potential for injuries is very real - they may not come to pass BUT THEY MAY. I just do not understand how an intelligent person as yourself cannot admit to the obvious facts. потому что Бог хочет это тот путь
Nothing. The claim was denied. Nobody, including the patient, is paying anything for it. You mean nobody pays for services rendered? потому что Бог хочет это тот путь
We conclude that Armey and Hall have suffered injuries in fact from their reduced private insurance. They have shown causation because their private insurance has been curtailed as a direct result of their legal entitlement to Medicare Part A benefits. And as to redressability, plaintiffs claim that they could obtain additional coverage from their private insurance plans if allowed to disclaim their legal entitlement to Medicare Part A benefits. What do you not understand about the court determining that the plantiffs were indeed injured as they had claimed? потому что Бог хочет это тот путь
The provider. There is no reimbursement for denied claims.
What do you not understand about the difference between a ruling on a motion to dismiss and a finding of fact at trial? They LOST. The District Court granted summary judgment. The Appeals court upheld.
Nobody pays the provider anything for denied claims.
The potential for injuries is very real - they may not come to pass BUT THEY MAY. I just do not understand how an intelligent person as yourself cannot admit to the obvious facts. If you choose to use an opt-out provider, your private insurer will not volunteer to pay the opt-out providers bill. I do not understant how an intelligent person, such as yourself, cannot see the obvious fact that the District Court (the trial court) granted SUMMARY JUDGMENT, and the Appeals Court UPHELD. Plaintiffs were denied rehearing and cert. You may see any injury you choose, you will have no case to take to court. These plaintiffs did not survive Summary Judgment. HALL v. SEBELIUS, 770 F. Supp.2d 61 (D.D.C. 2011) MEMORANDUM OPINION ROSEMARY M. COLLYER, District Judge. Plaintiffs are trapped in a government program intended for their benefit. They disagree and wish to escape. The Court can find no loophole or requirement that the Secretary provide such a pathway. Defendants' Motion for Summary Judgment [Dkt. # 42], which was previously denied without prejudice, is reconsidered and will be granted and Plaintiffs' Motion for Summary Judgment [Dkt. # 51] will be denied. A memorializing Order accompanies this Memorandum Opinion.
The provider. There is no reimbursement for denied claims. Every provider that I know of requires the patient to be responsible for payment over what the insurance entity pays. Almost all, if not all, providers either verify that the patient's insurance authorizes the procedure BEFORE hand and has the patient sign an acknowledgement of financial responsibility. Ex. genuine emergency procedures practically no provider will provide a service without having a financially responsible entity acknowledging responsibility for payment. потому что Бог хочет это тот путь
They lost on what the judge identified as the "merits" not the fact that the plantiffs were injured. The judge ruled that their injury was really but irrelevant to the "merits" of the case. потому что Бог хочет это тот путь
My private insurer most certainly will as long as that provider is in its "network" but will limit what it pays to the Medicare established amount. Yes, the plantiffs did lose EVEN THOUGH they were injured by have Medicare eligibility mandated on them with no way out. You keep posting the same quote which clearly shows that the case was decide on the basis of what the judge deemed to be the merits, namely: "Plaintiffs are trapped in a government program intended for their benefit. They disagree and wish to escape. The Court can find no loophole or requirement that the Secretary provide such a pathway." The decision was not based on the fact that the plantiffs were injured but on the basis that Congress and the President wanted it that way and left no way out for the plantiffs. In other words, screw you plantiffs, yeah, you are injured but that is what the government wants for you, so STFU and go away. потому что Бог хочет это тот путь
Which they cannot do for a Medicare patient.
They lost on SUMMARY JUDGMENT. The Plaintiff's case was dismissed on a pre-trial motion. It did not survive to even get to trial. The case was thrown out as a matter of law. Black's Law Dictionary, 6th Ed. Federal Rule of Civil Procedure 56 permits any to a civil action to move for a summary judgment on a claim, counterclaim, or cross-claim when he believes there is no genuine issue of material fact and that he is entitled to prevail as a matter of law.
My private insurer most certainly will as long as that provider is in its "network" but will limit what it pays to the Medicare established amount. That's what I said. On my MRI billed at ~$2,000, Medicare allowed ~$200. A private insurer will not pay the $2,000. It will pay its designated percentage of the $200, minus any applicable deductible. If you use an opt-out provider, you will be billed the $1,800 and maybe some more.
Then why are you arguing with me as this is exactly my point. The plantiffs suffered injury exactly because they could not escape the limits imposed by Medicare. The judge acknowledged that.
The judge acknowledged that.
"They claim they would receive enhanced coverage from their private insurers if they were not entitled to Medicare Part A benefits. For purposes of the standing inquiry, we must accept those declarations as true.
[quoting nc #14] It is only for purposes of standing inquiry that the court must accept the allegations as true.
Quoting the Opinion of the U.S. Supreme Court in Warth v. Seldin.
#39. To: nolu chan (#38)
The limits were on what the doctors could charge.
#40. To: SOSO (#32)
The fact is Congress tied SS to Medicare
#41. To: SOSO (#39)
I just retired and Medicare A is now my primary for hospitalization and our private insurance secondary. I have not enrolled in Medicare B so my private insurance is still primary for these service.
#42. To: nolu chan (#41)
As for docs who do not participate in Medicare (not a penny acceptance of Medicare funds) you should be able to use your private insurer or money. In general, those providers would be expensive.
#43. To: SOSO (#42)
You missed the whole point of this thread. Upon retirement you automatically become eligible for Medicare A. As a result your private insurance only covers the amount that is determined by Medicare A, even though the day before it was covering a higher amount for you when you were not eligible for Medicare A. You lose coverage. You have to pay more out of pocket.
#44. To: nolu chan (#11)
#45. To: nolu chan (#43)
No, Medicare becomes your primary insurer and pays most of the cost and yor private insurer become secondary and pays the remainder.
#46. To: SOSO (#16)
(Edited)
Total BS. Courts have the duty to determine what allegations have merit and what do not. Otherwise again BS allegation must be accepts for the purpose of standing. The court is not bound to accept every allegation for the purposes of standing.
#47. To: goldilucky (#46)
The only duty the Courts have is to determine three things: 1)personal jurisdiction over you, jurisdiction to hear your case, and finally standing to sue not just based on the merits of your case alone.
#48. To: SOSO (#47)
(Edited)
#49. To: goldilucky (#48)
For purposes of the standing inquiry, we must accept those declarations as true. [Emphasis added here]
#50. To: SOSO (#49)
(Edited)
#51. To: SOSO (#45)
Only up to the amount established by Medicare which I believe is less than what the private insurers pay when they are primary. The net result is that your out of pocket expense increases.
#52. To: nolu chan (#51)
An MRI had charges submitted by the imaging center for $2,214.00.
#53. To: nolu chan (#51)
Negative. The amount the provider can charge decreases to what Medicare allows.
#54. To: goldilucky (#50)
The reason why is that the judges in this matter relied on the Plaintiff's sworn Declarations that were attached to the Verified Complaints
#55. To: nolu chan, goldilucky (#51)
When the provider participates in Medicare..........
#56. To: nolu chan (#51)
I will provide my personal info from April. The figures come straight off my BCBS paperwork.
#57. To: SOSO (#52)
Where did you get an MRI billed for only $2,214?
#58. To: SOSO (#53)
So you are claiming that the plantiffs lied about having to pay more when Medicare became primary?
#59. To: nolu chan (#51)
#60. To: nolu chan (#58)
No, I am saying you are mistaken about what plaintiffs claimed.
#61. To: SOSO, goldilucky (#55)
If my provider of choice does not accept Medicare but had a separate agreement with the insurance company the insurance company would in almost all cases pay more for that provider's service than the Medicare amount. When I then become locked into mandated Medicare the insurance company automatically reduces what it will pay my provider of choice for a particular service. So when I now again go to my provider of choice I will have to pay more out of pocket if I want treatment by that provider. My alternative is to find another provider that accepts Medicare. It's Obama's lie again....
No matter how you cut it Big Brother is forcing us to take Medicare whether we like it or not. Only the wealthy (including the lawmakers) will be able to afford the provider of their choice and there will only be room for a few them.
Again I ask you, is this what you believe that the Founding Fathers intended?
#62. To: SOSO, goldilucky (#60)
ROSEMARY M. COLLYER, District Judge.
MEMORANDUM OPINION
II
ORDER
#63. To: SOSO (#59)
When Medicare is primary and private insurance secondary, what do the private insurers cover when Medicare denies a claim?
#64. To: SOSO, goldilucky (#60)
OK, please tell me what injury did they claim?
#65. To: nolu chan, goldilucky (#61)
If you choose not to accept Medicare Part A benefits, that's your choice. It will cost you a small fortune to use an opt-out provider. You should find out for absolute certain what your private insurer would pay. A mistake could be very, very expensive.
#66. To: nolu chan (#63)
When Medicare is primary and private insurance secondary, what do the private insurers cover when Medicare denies a claim?
#67. To: nolu chan (#62)
Plaintiffs' alleged injury is being forced to either (1) have inferior insurance foisted upon them, thereby precluding their ability to be covered by superior insurance; or (2) receive their superior non-Medicare Part A insurance at the cost of relinquishing their Social Security Retirement benefits, and re-paying past benefits received. Plaintiffs ask the Court to remedy this injury by invalidating the internal regulations that dictate this untenable choice — internal regulations which Plaintiffs claim are in contravention of the Social Security Act and the Medicare Act. Assuming this to be the case, the Court would have the power to invalidate those contravening regulations, thereby providing Plaintiffs with the redress they request.
#68. To: SOSO (#66)
You mean nobody pays for services rendered?
#69. To: SOSO (#67)
What do you not understand about the court determining that the plantiffs were indeed injured as they had claimed?
#70. To: SOSO (#66)
You mean nobody pays for services rendered?
#71. To: SOSO, goldilucky (#65)
It took you a while but thanks for seeing the light. Yes, if my current providers of choice do not accept Medicare then we will be injured in one of two ways or perhaps both. First, if I chose to continue with THE PROVIDER OF MY CHOICE WHICH I HAD BEFORE MEDICARE WAS FORCED UPON ME I will have to pay more, perhaps more than I can afford OR I will have to chose a provider of lesser quality as we judge that.
V. CONCLUSION
#72. To: nolu chan (#68)
You mean nobody pays for services rendered?
#73. To: nolu chan (#69)
They LOST.
#74. To: nolu chan (#71)
If you choose to use an opt-out provider, your private insurer will not volunteer to pay the opt-out providers bill.
#75. To: SOSO (#72)
Every provider that I know of requires the patient to be responsible for payment over what the insurance entity pays.
#76. To: SOSO (#73)
They lost on what the judge identified as the "merits" not the fact that the plantiffs were injured.
Summary judgment. Procedural device available for prompt and expeditious disposition of controversy without trial when there is no dispute as to material fact or inferences to be drawn from undisputed facts, or if only a question of law is involved. (citation omitted)
#77. To: SOSO (#74)
If you choose to use an opt-out provider, your private insurer will not volunteer to pay the opt-out providers bill.
Top • Page Up • Full Thread • Page Down • Bottom/Latest
[Home] [Headlines] [Latest Articles] [Latest Comments] [Post] [Mail] [Sign-in] [Setup] [Help] [Register]
